Comprehensive Approach to theManagement of Scapular Dyskinesiain the Overhead Throwing Athlete
- By Chris Vendilli
- •
- 13 Apr, 2018
- •
This is a subtitle for your new post

SM is a 16-year-old right-handed female volleyball player with no significant medical history who presents with progressively worsening right shoulder pain localized to the right periscapular region. There is no associated trauma or inciting event and pain is exacerbated when she serves or spikes the ball, and typically alleviated with rest. She denies any neck pain, radicular symptoms in the arm, or focal weakness, but her right arm just feels weaker, with less velocity on her serve.
Treatment has included rotator cuff strengthening exercises and modalities under the supervision of her athletic trainer, but no physical therapy or injections. She was evaluated by her PCP, who ordered routine x-rays of the right shoulder that were normal. She also states that her PCP noticed her right shoulder blade was sticking out a little, so she underwent an electrodiagnostic evaluation that was negative.
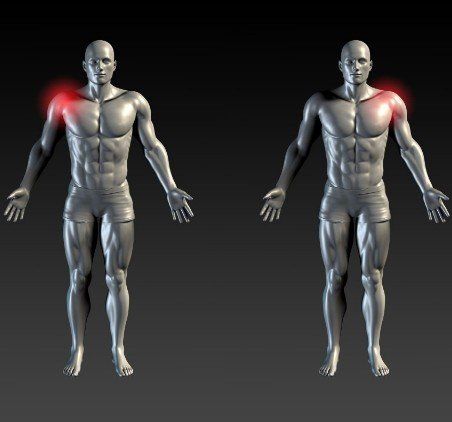
Upon examination at the UPMC Sports and Spine Clinic, she demonstrates slightly increased cervical flexion and forward rounded shoulders. The right scapula is malpositioned with increased prominence of the infero-medial angle. She has full active shoulder range of motion with the exception of pain-limited abduction to 130 degrees and
flexion to 150 degrees (see Figures 2a, 2b, 2c, above). She is tender to palpation along the medial border of the coracoid
process, but otherwise there is no tenderness in the shoulder or cervical spine. Her neurologic and musculoskeletal examination is otherwise unremarkable, with the exception of decreased right hip internal ROM. She is frustrated because she doesn’t know what is wrong and all tests to date have been normal. Now with the volleyball season over, she is looking forward to playing spring softball as an outfielder and is asking for recommendations.
Click here to download the complete paper.
A 35-yr-old right-handed male dishwasher was referred to the authors’ electrodiagnostic laboratory for evaluation of left shoulder weakness and atrophy. The patient reported the insidious onset of a sharp, “stinging” pain of his left shoulder region 6 mos before evaluation. This pain lasted approximately 10 days and gradually subsided after initiation of ibuprofen prescribed 1 wk after onset. He denied any preceding systemic illness or trauma, associated neck or radicular pain, and no weakness or numbness/tingling. A few weeks after resolution of the shoulder pain, he noted progressive weakness and decreasing muscle bulk of his left shoulder. His medical history was otherwise unremarkable, and he was taking no medications.
Upper extremity inspection revealed significant atrophy of the entire left deltoid with otherwise normal upper extremity muscle bulk. The findings from the neurologic examination were normal except for slightly weak shoulder abduction and flexion on the left with diminished sensation of a small area overlying the left deltoid.
Magnetic resonance arthrogram of the left shoulder showed significant atrophy and edema of the left deltoid muscle as well as a superior labral tear and minimal undersurface fraying of the rotator cuff.
Neuralgic amyotrophy (also known as Parsonage-Turner syndrome) is a neurologic syndrome affecting the brachial plexus. Clinically, it is characterized by the acute onset of intense pain with resolution in 1–2 wks followed by weakness and atrophy of the arm/shoulder girdle muscles. Sensory loss in the axillary nerve distribution is common. Neuralgic amyotrophy may have an antecedent triggering event, such as a viral illness, immunization, pregnancy, or surgery; however, as in this case, an inciting etiology is frequently not identified. Although most cases present with unilateral findings, bilateral involvement may occur. Discrete mononeuropathies (e.g., suprascapular, long thoracic, or axillary nerve) are relatively common (6%–41%). Recovery may require up to 2–3 yrs.
Click hereto view the full article